
Corneal transplantation surgery may be necessary for those with corneal disease or significant scarring to the clear front surface of the eye. This surgery is also known as a keratoplasty procedure and can benefit patients by once again giving them a more regular and transparent surface.
A transplant often becomes necessary when a particular organ/tissue becomes damaged beyond repair. The damaged area is replaced with healthy donor organ/tissue. Corneal transplantation, can also be known as keratoplasty surgery, and is the most successful transplant procedure performed worldwide. This is largely due to the fact that corneal tissue does not have to be “matched” between donor and recipient. In other words, a healthy cornea may be donated to any individual with good chances for success. Donor tissue is stored and ordered from an Eye Bank. Vision can be greatly improved if the procedure is successful and healing occurs without problems. Keratoplasty corneal transplants are very common in the United States with annual procedures exceeding 40,000. Fortunately, enough donor tissue usually exists to keep up with the demand, meaning there is usually no waiting time for tissue like many other organ transplants.
If the front surface of the eye is scarred or the shape is abnormal, vision is limited and may not be able to be corrected with glasses or contact lenses. Corneal transplants are performed for a variety of reasons that include corneal disease, injuries and swelling that will not resolve. Keratoconus corneal transplants are most commonly performed on younger patients in the first 3-4 decades of life. Most of the other disease conditions will become more prevalent as a person ages. Listed below are some of the most common reasons to perform a keratoplasty:
There are three basic keratoplasty types and they are used for specific conditions. Penetrating keratoplasty is used for corneal disease that has impacted the front part of the cornea. DALK or deep anterior lamellar keratoplasty can be done for the same conditions as a penetrating keratoplasty. DSAEK or Descemet’s stripping automated endothelial keratoplasty and DMEK, Descemet’s membrane endothelial keratoplasty are done for endothelial disease such as Fuch’s endothelial dystrophy.
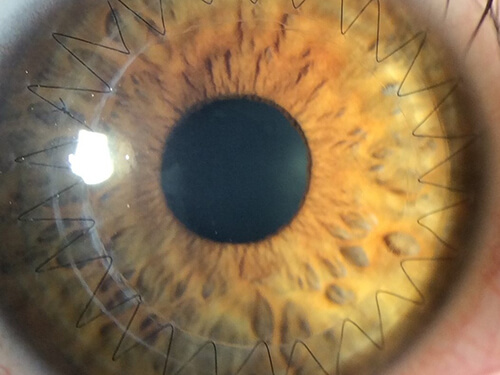
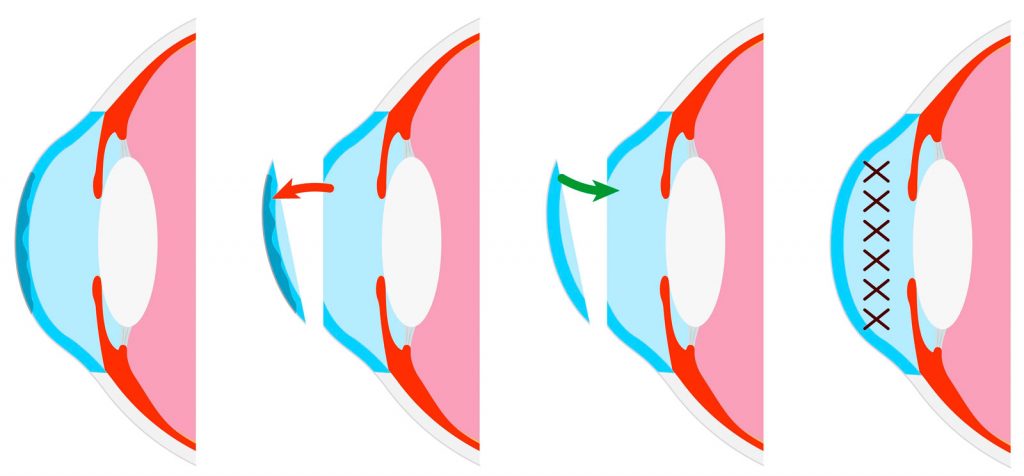
The Penetrating Keratoplasty procedure (or PKP/PK) is a full-thickness or all five layers of the cornea replacement operation. Patients who undergo a PK have structural damage to several anterior layers of the cornea. Sutures are placed and the healing time for restoration of vision can be a year or more after successful transplantation of tissue.
There are 4 types of partial-thickness corneal tissue corneal transplants. There are three anterior graft technique: Descemet’s Stripping Endothelial Keratoplasty ( DSEK ), Descemet’s Stripping Automated Endothelial Keratoplasty ( DSAEK ), and Descemet’s Membrane Endothelial Keratoplasty (DMEK). There is one partial-thickness “ anterior “ corneal transplant procedure and it is termed Deep Anterior Lamellar Keratoplasty ( DALK ).
DSAEK, Descemet Stripping Automated Endothelial Keratoplasty) is a less invasive corneal transplant surgery technique. It is done when only the posterior or endothelial surface of the cornea is diseased. It is used when the endothelium no longer functions. The most common cause is an inherited disease called Fuch’s Endothelial Dystrophy. Endothelial keratoplasty or EK is termed a partial posterior transplant of tissue. The tissue is inserted through a small incision and no suturing is required.
A corneal transplant procedure typically takes between 30 minutes to 2 hours. Pre-operatively you will be given sedatives and a local anesthetic. During the procedure, you will be awake, but comfortable. Your surgeon will use a high-powered microscope throughout the procedure. Your surgeon will use a lid guard to keep the eye open. Numbing medications will help so you feel nothing during the procedure. Only the diseased, scarred or damaged cornea will be removed and replaced with keratoplasty eye surgery. Healthy donor tissue matched for the replacement area will be obtained and placed. With DSAEK surgery an air bubble will keep the tissue in place. With a penetrating keratoplasty the tissue must be sown in place. The sutures usually stay in place for 1 year. A protective shield will be placed over the eye socket for safety while asleep for a week or so.
It is important that you adopt the right self-care practices after surgery to get the best possible outcome and highest corneal transplant success rate. Corneal transplant surgeons can share their personal corneal transplant results but can not guarantee 20/20 vision after corneal transplant surgery.
Here’s what to keep in mind to preparation for successful recovery after your corneal transplant procedure:
In determining who is a good candidate for a corneal transplant, the patient must be evaluated with a complete eye examination. Patients are considered suitable if they have vision loss from significant corneal disease or damage. With consideration for transplant, social support for the patient is important to make sure the patient and support system are providing appropriate care for the graft to survive in a healthy fashion. During the examination several tests will be determined beyond level of vision. These tests frequently involve a slit lamp examination, corneal topography, corneal tomography, corneal thickness, optical coherence tomography, keratometry and evaluation of overall health, systemic conditions and any other eye diseases beyond the cornea.
Our corneal transplant surgeons have decades of experience in performing corneal transplants with the goal of restoring and preserving your vision and allowing for a fully active lifestyle.
Corneal transplant procedure techniques include full-thickness / penetrating keratoplasty ( PK ), artificial corneal transplant of acrylic cornea also known as keratoprotheses, and partial thickness transplants which include Descemet’s stripping automated keratoplasty ( DSAEK ), Decemet’s membrane endothelial keratoplasty ( DMEK ) and deep anterior lamellar keratoplasty ( DALK ).
Dr. John Doane and Dr. Stephen Stechshulte are fellowship trained cornea and refractive surgeons.
Corneal transplants are very common in the United States; about 40,000 are performed each year. While success rates may vary due to pre-existing conditions in your eye, technological advancements have increased your chance of success. Approximately 90% of corneal transplants are successful, and the new cornea will stay healthy for an average of 10 years. In the unlikely event that your surgery is not successful, or if your cornea does become cloudy again, you can always receive another transplant.
There are several milestones in corneal transplant procedures. Does the corneal graft take? Does the body reject the tissue? Can the graft fail early or late? Does a failed graft need to be replaced? All of these issues need to be answered with time. There are issues early that need to be understood. Infections can occur and usually are treated successfully. Graft acceptance and survival are the key early considerations. Bleeding and loss of vision can occur during a procedure. Experience of the surgical team can lessen or nearly eliminate most issues and with proper care and follow-up your best chances for success can be realized.
The average corneal transplant can last over a decade and if there is a good tissue match some grafts have been known to last many decades. If a graft fails at some point another, corneal transplant can be performed.
As with any surgery complications can arise. The procedure itself is considered safe. Many patients do not have a choice if their vision is poor, the only thing that can help them is a corneal transplant. So, the benefit of vision improvement has to exceed the risk of vision loss or complete loss of sight. Your care team will review and inform you of the risk, benefits and alternative to treatment or no treatment.